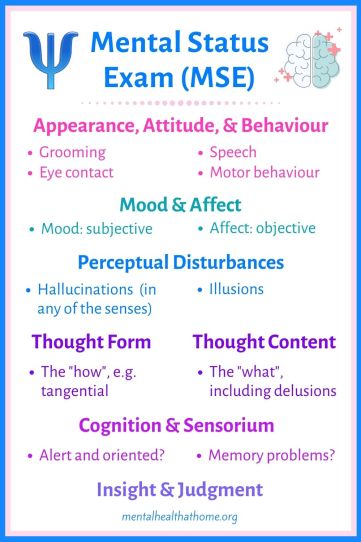
The mental status exam (MSE) is a framework for assessment that’s used widely in the field of psychiatry. Rather than being a one-time assessment, it is used on an ongoing basis to capture how a patient is doing on any given encounter (and I use the term patient to describe the role and not the person as a whole). This is what it covers.
For more on some of the terms used in this post, check out the glossary of psychiatric terms.
Table of Contents
Appearance, attitude, and behaviour
This part of the MSE isn’t supposed to be about passing judgment; instead, the purpose is to identify clues that could potentially give information about someone’s mental health.
Apparent vs stated (i.e. actual) age
“Stated age” refers to actual age, as stated in the chart, and isn’t meant to imply that someone is lying about their age.
Grooming
Assessment of grooming is most useful when the clinician has something to compare it to, whether that’s previous documentation or the patient’s baseline that they’re aware of. The key here is to look for anything that’s indicative of the person’s mental state.
Someone who’s manic may be dressed in a flamboyant or provocative manner, and may be wearing heavy makeup where they normally wear none. No one is manic simply because they’re wearing a miniskirt and bright makeup, but if you consider that in the context of the person also having pressured speech and sleeping 2 hours a night, that outward presentation is probably a clue.
Someone who’s depressed may not be showering often, and their hair and body odour may reflect that. They may not have changed clothes since that last shower.
Hygiene may also be an issue for people with schizophrenia. Outfits may be quirky with many layers that don’t really go together. Some people with schizophrenia may dress inappropriately for the weather. If you’re sweating because the air conditioning isn’t turned up high enough and the other person is dressed for a polar expedition, that’s a red flag.
Eye contact
This is another area where it’s useful to be aware of the patient’s baseline as well as relevant cultural norms. When I’m very depressed, I make minimal eye contact, which is characteristic of psychomotor retardation. It’s also common for autistic people to make limited eye contact. Someone who is paranoid may have a wide-eyed, unblinking gaze.
Cooperation with interviewer
Someone may be “guarded” (reluctant to reveal information) due to paranoia, or rapport may be “tenuous” (weak) because the interviewer is a pompous jerk, and this can mean the information gathered through the interview isn’t necessarily reliable and therefore the assessment may not accurately capture the entire clinical picture.
Motor behaviour
There are a variety of ways in which mental illness can affect people’s physical activity. For example, mania may speed up people’s movements (psychomotor agitation), while depression may slow it down (psychomotor retardation). Catatonia refers to extreme disruptions in motor behaviour.
Medication side effects may also be visible, including tremor and tardive dyskinesia (involuntary movements).
Speech
This includes rate, rhythm and volume, as well as amount of speech. Someone with schizophrenia may have alogia, also known as poverty of speech. If someone gives brief responses to questions but otherwise doesn’t speak, that might be referred to as having limited spontaneous speech.
If someone is slow to give answers to basic questions they may be described as having “latency of response.” This can be reflective of the thought process, or it may have a motor component, as is seen with psychomotor retardation in depression.
People with mania often have “pressured speech,” which is rapid and difficult to interrupt.
Mood and affect
Mood is how the patient describes their emotional state, and affect is the emotional expression visible on the patient’s face. Labile mood changes rapidly.
Diminished affect may be described as restricted, blunted, or flat, with flat being the most extreme. Affect may also be referred to as incongruent if, for example, someone was laughing while speaking about a very sad topic or talking about their depressed mood.
Perceptual disturbances
Perceptual disturbances are a key area of the mental status exam for anyone who might potentially be experiencing psychosis. Perception of the self in relation to the environment may also be altered in people who are experiencing depersonalization and derealization.
Hallucinations
Hallucinations are internal stimuli rather than external stimuli that come from the outside world. Auditory hallucinations are most common, but visual, tactile, olfactory smell), and gustatory (taste) hallucinations may also occur.
Illusions
These are skewed perceptions of stimuli that actually do originate in the external environment.
Thought form/thought process
This part of the mental status exam considers the “how” of a person’s thinking. Is it logical? Is it disorganized? Thought form isn’t assessed based on asking the patient specific questions, but rather is evaluated based on the entirety of the interview.
Circumstantiality is sort of like beating around the bush; there’s some meandering along the way, but eventually, the point is reached. Tangentiality goes off in another direction without returning to the original point. Loose associations or derailment involves thoughts that aren’t connected at all.
There can also be poverty of thought, which is along the lines of “the lights are on, but nobody’s home.”
Thought content
This considers the “what” of a person’s thinking, and may include delusions, obsessions, or suicidal or homicidal ideation (commonly abbreviated as SI/HI).
Common types of delusions include grandiose, persecutory, jealous, somatic, or guilty. Ideas of reference involve interpreting special messages toward oneself from the external environment, such as from tv or radio. Delusions of control include thought insertion (thoughts being put in one’s head), thought withdrawal (thoughts being plucked out of one’s head), and thought broadcasting (believing one’s thoughts can be heard by others).
Cognition and sensorium
This includes things like orientation, concentration, and memory. Further formal testing may sometimes be required. A brief test like the Montreal Cognitive Assessment (MOCA) or Folstein Mini Mental State Exam (MMSE) includes basic questions like what day/month/year it is, spell “world” backwards, subtract by 7’s (“serial sevens”), remember 3 objects, and copy a geometric design.
Baseline intelligence (IQ) and education are relevant here; if someone with no formal education can’t subtract by 7’s, that doesn’t necessarily indicate there’s a problem, but if an astrophysicist can’t do that task, it’s a pretty good indicator of impairment. If you’ve got someone (like me) who has learned the test enough to spell d-l-r-o-w with as little thought as w-o-r-l-d, that question isn’t going to elicit a meaningful answer.
Insight and judgment
Insight refers to the patient’s level of awareness of the symptoms they’re experiencing and the impact those symptoms are having on their functioning. Lack of insight is referred to as anosognosia.
Insight tends to be poorer with some illnesses compared to others, and it may fluctuate depending on the severity of the symptoms someone’s having at any particular time. Someone may have good insight into the symptoms they’re experiencing and still disagree with the clinician on the cause of those symptoms or what should be done about them.
Judgment refers to the extent to which a person’s judgment, particularly with regard to behaviour, is influenced by the symptoms they’re currently experiencing. An obvious example of poor judgment would be someone who was manic blowing a bunch of money at a casino.
The overall picture
The MSE is a basic building block of psychiatric assessment. Some clinicians are better than others at eliciting information, and some are more likely to jump to conclusions than others. The MSE is supposed to be based on clinical assessment rather than personal judgment, but even when it’s not influenced by passing judgment, the language used can come across that way if people aren’t familiar with it and reading their own charts. But don’t hesitate to ask questions. Something that looks awful might have a good explanation behind it. So go ahead and ask.

Making Sense of Psychiatric Diagnosis aims to cut through the misunderstanding and stigma, drawing on the DSM-5 diagnostic criteria and guest narratives to present mental illness as it really is.
It’s available on Amazon and Google Play.

Really interesting, thanks.
Even knowing what the professional is guiding their assessment on, I bet I still can’t do eye contact well enough!
But chances are there’s naturally a difference in your eye contact when you’re really low and when you’re doing well.
Definitely.
“The astrophysicist can’t subtract by 7s.” Just became my new anxiety tagline.
Very interesting, thank you.
Very interesting! Thanks for sharing. I liked how you mapped out how some of these traits manifest with you when you are depressed. I definitely stopped to consider the same, gives me good insight! And it can help me in my work with my students too.
Nice breakdown!
Thanks!
thats interesting! I’m not sure we have that but we probably have something similar to it here in ireland. Interesting to see how other countries do things!
According to a quick Google search, yes, it’s part of psychiatric training in Ireland. As a patient you wouldn’t necessarily know it was being used since it’s more a framework to organize assessment rather than a specific test.
I’ve been seeing my psychiatrist for almost 13 years. He always said that he takes careful note of his very first observations of me when he opens the waiting room door, to my walk down the hall to his office, to me sitting down, and onward. I always feel bad when people say they have psychiatrist appointments via video. I think that’s a bad trend, though I understand for some there are too few doctors available in their area.
I agree.
I loved this post Ashley and will save same to revisit down the line lol – you are doing great work getting all this together and sharing and I hope lets of the work is therapeutic for you