
Wouldn’t it be nice if the treatment of depression was simple? Unfortunately, there’s nothing simple about depression treatment in the real world. Treatment-resistant depression (TRD) refers to depression that hasn’t responded to trials of adequate duration and dosage of at least two antidepressants.
When determining whether the illness is treatment-resistant, it’s important to consider whether previous medication trials have been long enough that you’re actually seeing the therapeutic effect (or lack thereof) and not just side effects. For people who do experience treatment resistance, it may be that treatments that were trialled didn’t work in the first place, or it may be a matter of meds that previously worked but are no longer doing the job. You can read more about the latter in the post Why Do Psych Medications Stop Working Sometimes?
This post will look at some of the options for dealing with treatment-resistant depression, and I’ll also talk about my own experience living with it.
What the STAR*D study tells us
STAR*D (Sequenced Treatment Alternatives to Relieve Depression) was a large study conducted under real-world conditions. While a lot of studies measure response to treatment (response is typically considered to be a 50% reduction in symptom scores), STAR*D used remission (near-absence of syndromes) as an endpoint. While it’s not always possible to achieve remission, it should be the goal that’s aimed for, as people who can get into remission have better long-term outcomes.
STAR*D had four levels of treatment that participants moved through if they weren’t responding to treatment.
- Level 1: the SSRI citalopram
- Level 2: patients were offered a choice of psychotherapy, switch to another antidepressant (bupropion, sertraline, or venlafaxine), or augmentation of citalopram with either bupropion or buspirone
- Level 3: patients were offered a choice of switching antidepressant (to mirtazapine or nortriptyline) or augmenting with lithium or liothyronine
- Level 4: patients were randomly assigned to switch to either the monoamine oxidase inhibitor (MAOI) tranylcypromine (Parnate) or the combination of venlafaxine plus mirtazapine
Only about 1/3 of people get well with a trial of one antidepressant, and a further 1/4 get well with a trial of a second antidepressant. After four medication trials, 33% of people still hadn’t gone into remission. That’s a whole lot of people who aren’t getting well.
Diagnostic clarification
If depression isn’t responding to treatment, it’s important to reevaluate the diagnosis. A key question to consider is whether the issue may be bipolar rather than unipolar depression. Antidepressants don’t work that well in bipolar disorder, and mood stabilizers play a much more important role.
If there’s a co-occurring psychiatric disorder, like borderline personality disorder or PTSD, that could be feeding into the depression, it’s important to make sure those other conditions are being appropriately treated.
It’s also useful to consider whether there might be a medication (e.g. a corticosteroid), medical condition (e.g. hypothyroidism), or substance use that could be contributing to the problem.
Strategies for treatment-resistant depression
Switch up the treatment
Let’s say the diagnosis is major depressive disorder and no complicating factors have been identified. Have you tried psychotherapy? If not, that’s always a great place to start. Other first steps might be to increase the dose, switch antidepressants, or try antidepressant combos.
Antidepressant augmentation
Augmentation is another strategy. It involves adding medications to an antidepressant regimen to achieve a greater therapeutic effect.
Options include the mood stabilizer lithium, atypical antipsychotics, and liothyronine (Cytomel), which is the T3 form of thyroid hormone. Stimulants like dextroamphetamine are sometimes used for augmentation.
Ketamine/esketamine
Ketamine, a dissociative anesthetic, has a novel mechanism of action, affecting the glutamate system in the brain. It works rapidly, but it wears off after a week or so. It’s a relatively new treatment and availability can be limited, but there’s some good research supporting its effectiveness.
While ketamine is administered by IV infusion, esketamine (Spravato) is available as a nasal spray. Ketamine contains two mirror-image molecules, R- and S-ketamine. Esketamine only contains the S-ketamine molecule.
You can find out more in the post Ketamine for Treatment-Resistant Depression.
Try novel medications
Ok, so what if you’ve tried, maxed out, and failed on standard medication options? It may be time to start reaching a little further afield for options that haven’t been as well studied.
Botox
Botox (botulinum toxin) may seem like an odd choice for depression, but a few small studies have found that injecting Botox into the frown line areas on the forehead actually led to an improvement in depressive symptoms, even in people with treatment-resistant illness. The thinking behind it is that not only does facial musculature express mood states, but it gives feedback that in turn regulates mood states. By preventing frowning, Botox may disrupt that harmful feedback loop.
For cosmetic purposes, the effects of Botox last about 3-4 months, although in the studies for depression, the beneficial effect was found to last even longer.
I tried two rounds of Botox, getting 29 units each time, which was the amount used in the studies I found. After a few days, I started noticing a feeling that I would describe as numb but not numb. I could still feel touch and pressure, but when I tried to move the muscles in my forehead, I got a numb sort of feeling. I had no idea how much I had been frowning until after I got Botox and was unable to frown anymore.
Did it help with my depression? I would say a cautious maybe, but the effect wasn’t significant enough that it seemed worth continuing to pay for.
Anti-inflammatories
There are a number of other drugs that have been studied that are potential options although there isn’t a large body of research evidence to support them. D-cycloserine is an antibiotic that at high doses acts on the same NDMA receptors that ketamine works on. Minocycline is another antibiotic that has shown some benefit, as it calms inflammatory microglia in the brain.
Infliximab (Remicade), normally used for autoimmune diseases, has shown some antidepressant effect in depressed people with elevated levels of inflammation. As a biological agent, it is quite expensive.
Scopolamine
The cholinergic system is another potential target. Scopolamine, also used for nausea, appears to have an antidepressant effect via its action on muscarinic receptors in the brain.
Studies have primarily involved 3 doses via IV infusion, with a rapid but not sustained effect. This is something I’ve considered trying in the form of an intramuscular injection, as the oral version of scopolamine that’s available in Canada doesn’t cross the blood-brain barrier to enter the brain.
Kappa opioid blockers
Blocking kappa-type opioid receptors has been associated with an antidepressant effect. This is different from the µ-type opioid receptors which are associated with effects like analgesia and respiratory depression.
Buprenorphine, which is found in Suboxone, is a kappa antagonist, but it also has effects on µ receptors, and research is being done to develop drugs that are selective for kappa receptors with no activity at µ receptors.
Add supplements
There are a number of over-the-counter supplements that have shown some effectiveness in depression, and you can try adding them on to a medication regimen. These include L-methylfolate, which may be most useful in those with elevated inflammation or impaired methylation cycles, S-adenosyl methionine (SAMe), omega-3 fatty acids, creatine, and n-acetyl cysteine, which decreases oxidative stress. There’s more on this in the post Supplements for Depression that Actually Work.
I take L-methylfolate along with vitamin B12 by injection every 2 weeks, and I’ve noticed that if I go longer than 2 weeks between shots, my thinking and my energy start to slow down. I also take omega-3’s, although I’m not sure if it’s actually helping me or not.
Somatic treatments
Another approach to treatment-resistant depression is somatic treatments, which stimulate electrical activity in the brain. The post Somatic Treatments for Depression goes into more detail, but here we’ll briefly cover the most common options, ECT and TMS.
ECT
Probably the best known is electroconvulsive therapy (ECT). It involves stimulation with an electrical current to produce a seizure. This is done while under anaesthetic, and a muscle relaxant (succinylcholine) is used so there isn’t a physical seizure. It’s a highly effective treatment, and there’s nothing barbaric about it, despite popular misconceptions.
I’ve had several courses of ECT in the past, and it’s been quite helpful for me. You can read more about my experiences in the post This One Flew Over the Cuckoo’s Nest: ECT in Real Life. It’s something I’ve wished I could access on an outpatient basis, but because of the anaesthetic, you’re required to essentially have a babysitter on ECT days, which just isn’t logistically feasible for me.

TMS
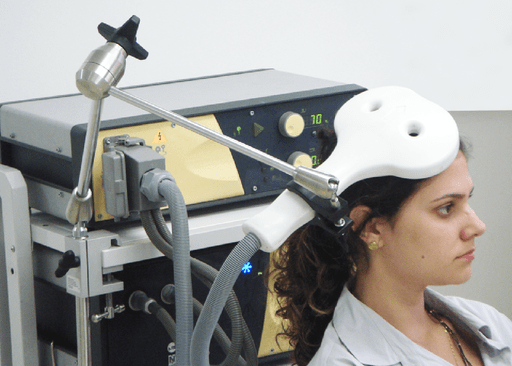
Another option is transcranial magnetic stimulation (TMS), which uses a magnetic field to stimulate the brain. It has demonstrated good results in research studies, although it’s not as effective as ECT. Because there’s no anaesthesia involved, it’s much easier to do in the community than ECT. Treatments are typically five days a week for six weeks.
Living with treatment-resistant depression
I used to have periods of full remission between episodes of illness, but recently, my depression has become increasingly resistant, despite taking two antidepressants with multiple medications for augmentation. My med cocktail still works for some symptoms, but no longer does much at all for others.
What meds still do help with
The meds really don’t touch the anhedonia, but they do help with my mood. The mental pain that I associate with my depressed mood is less, and guilt and irritability don’t tend to be issues when I’m well-medicated. Guilt doesn’t tend to be an issue for me when I’m fully well, but when my depression is bad and I’m un-/under-medicated, it’s intense.
Active suicidal ideation isn’t generally an issue when I’m sufficiently medicated. Treatment resistance has brought a new baseline lack of desire to continue living, but that feels quite different from suicidal ideation. I do still get some flare-ups of suicidality, but I’ve never been impulsive in that sense and I know I can get through flare-ups, so they don’t concern me all that much when they do pop up.
I can’t sleep if I don’t have meds, but for the most part, it’s okay as long as I’ve got my quetiapine. My appetite disappears when my depression is really bad, but the meds usually help with that.
The meds help a bit with cognitive symptoms like poor concentration and memory, but those things are still major issues on an ongoing basis.
Where the wheels really fall off is in terms of psychomotor retardation (slowing of movement and thoughts). I have ongoing significant psychomotor retardation even with meds, and that’s had a massive impact on my level of functioning. When I’m dealing with situation stressors, I get even slower.
Facing the future
Some of the treatments that I would like to try, like ketamine, just aren’t accessible at this point in time. It’s frustrating to know that there are options out there that could help, but they’re not available to me.
It’s definitely been a process to wrap my head around the idea that remission no longer seems like a possibility. Hope becomes harder to find when the treatments that are supposed to work just don’t.
How is your treatment working for you? If you have treatment-resistant depression, what other options have you considered?
References
- Finzi, E., & Wasserman, E. (2006). Treatment of depression with botulinum toxin A: a case series. Dermatologic Surgery, 32(5), 645-650.
- Magid, M., Reichenberg, J. S., Poth, P. E., Robertson, H. T., LaViolette, A. K., Kruger, T. H., & Wollmer, M. A. (2014). Treatment of major depressive disorder using botulinum toxin A: a 24-week randomized, double-blind, placebo-controlled study. Journal of Clinical Psychiatry, 75(8), 837-844.
- National Institute of Mental Health. (2016). Questions and Answers about the NIMH Sequenced Treatment Alternatives to Relieve Depression (STAR*D) Study — All Medication Levels.
- Wollmer, M. A., de Boer, C., Kalak, N., Beck, J., Götz, T., Schmidt, T., … & Sönmez, D. (2012). Facing depression with botulinum toxin: a randomized controlled trial. Journal of Psychiatric Research, 46(5), 574-581.

Managing the Depression Puzzle takes a holistic look at the different potential pieces that might fit into your unique depression puzzle.

I suppose I have that condition TRD. I’ve had depression since I was 13, over 45 years ago. I’ve been on most of the prescription anti-depressants, and none worked totally, but Zoloft has the best results (IMHO). I take that and a low dose of Trazadone (for insomnia) and the combination seems to keep me, if not joyful, at least not horribly depressed. I also consider therapy to be the best tool for combating the severe episodes, I see a therapist at least once a month, or more if I’m feeling down. I’ve talked about depression to other people (or blogged about it) and one thing is always consistent: No two people respond the same way to the same methods or drugs. So it takes a lot of patience to find out what is going to work, and work the best for any individual. Just my thoughts.
I’ve recently started following your blog and find it informative and encouraging. Thanks! 🙂
I’m glad you’ve found a combination approach that’s working for you 🙂
I have had hyperthyroidism since I was seven years old. It wasn’t diagnosed until I was ten. I have always struggled with depression but didn’t realise the two are linked? I take levothyroxine. I’m now 58. I am also autistic which throws anxiety into the mix as well.
Sorry if that sounds a bit stilted, I’m really tired today. Thanks for the post Ashley xx
Not stilted at all. Things can get so complicated when multiple different conditions are involved.
Your blog is just SO good, keep up the good work. I may try Ketamine. I have a good friend who became so depressed after her husband left her, that she was literally catatonic. Our church had a laying on of the hands, and she says she never, ever suffered one more depressive moment. Faith is healing as well. xoxo
Oh interesting.
I’ll add to consider ADHD, ASD or another developmental disorder that might be co-occurring. Also, consider that there might be a global chronic illness like fibromyalgia or EDS or another disorder that messes with pain signals or stress hormones and thus is known for co-occurring anxiety and/or depression. All of the above (plus trauma, of course) ended up being it for me. Folks with ADHD are less likely to respond to SSRIs genetically – my Genesight test reinforced that for me – and it’s really hard to treat the anxiety and depression that stem from ADHD until its underlying chaos and overwhelm is at least partially managed with appropriate medications. I couldn’t make any headway in therapy or with treating my depression or anxiety until I started stimulants for ADHD. They don’t fix the problem (any more than bipolar meds can truly “fix” bipolar), but they one of those medication strategies that are often so critical as a first-line treatment that nothing else really helps until you add them. ADHD is particularly likely to be missed in psychiatry in women and in those with the inattentive subtype.
Excellent points.
Wow…Ashley…looks like you are answering my questions today. I have had a lot of them for a long long time…n I am thrilled to know that answers exist!! Hugs
Oy. I’ve probably been depressed fairly consistently (bar occasional gaps of no more than six months, maybe one longer gap early on) for about twenty years, although I wasn’t diagnosed until 2003. I’ve been on LOTS of combinations of medications. I take omega-3 and zinc. I’ve tried various talking therapies (CBT, psychodynamic, I think others). At times I’ve been tempted to try ECT, but that hasn’t happened for various reasons.
I’ve just been referred to a psychiatrist again because of another relapse and this time I want to talk about alternative diagnoses. This has been done a bit in the past, but I’ve always been told I have straightforward unipolar depression, not bipolar disorder, autism, or anything else. I’m less and less convinced. So many of my friends and the people who read my blog who have experience of depression say that what I experience is so much worse than what they experience. I’m fairly sure I’m somewhere on the autistic spectrum (which wouldn’t directly cause depressive symptoms, but it would explain a lot about why I can’t get my life together and particularly why I’m socially anxious), but after two assessments, and despite a psychiatrist who insisted I was on the spectrum even though she never did a formal assessment, I’m sort of resigned to the fact that the psychiatrists won’t give me a piece of paper that says that I’m autistic. Bipolar doesn’t seem to fit, but I’m currently reading a book on complex PTSD which surprisingly seems to describe me well, but I’m worried that I’m reading too much into it. I periodically find something (an illness or syndrome) that seems to explain a lot and I get excited that I might finally have a breakthrough and then the mental health professionals shoot it down, despite the fact that they don’t have much of a clue about what could help me.
I suspect that C-PTSD is often overlooked as a cause of depressive symptoms, and I’d say the fact that it’s not even recognized yet in the DSM speaks to that.
Wow, I didn’t know that it’s not recognised in the DSM. I know the author of the book I’m reading thinks that most depressive and obsessive disorders have their origins in C-PTSD and even if that’s hyperbole, I can believe that it accounts for a lot of depression. I don’t think it has ever been raised as an issue for me before though, because my childhood traumas weren’t obvious ones. I only thought about it because I got talking to someone at my autism group who thinks that many autistic people have C-PTSD from the way they were treated as children. What she said seemed to describe me, although I still feel I was not traumatised ‘enough’.
Children are so much more vulnerable to stress it makes sense that it wouldn’t necessarily need a “capital T” trauma to cause lasting effects.
Yes, I’m beginning to realise that. I was in a situation that would probably have been upsetting for anyone, but as a young, sensitive and possibly autistic child it was just too much for me, especially as it went on for years.
Very interesting post. My friends and I were just talking about the botox being a means to help with migraines, never thought it would help with depression before.
I’ll have to check out the ketamine for when my depression gangs up on me again. Right now, it’s kept at bay. Thank goodness.
For sure
Good gosh! All those crazy treatments! I think I know of a better way treating depression…society.